The true identity of the world’s leading killer is high blood pressure. It is also a silent killer because, most of the time, there are no symptoms associated with it.
Can we prevent this killer from causing harm? Definitely yes. But this was not possible on April 12, 1945, the day Franklin D. Roosevelt, 32nd President of the United States, died of a massive cerebral hemorrhage. His blood pressure was > 300/190 at the time.
Roosevelt’s blood pressure had been elevated since at least 1935. At the time of his death, little was known about the treatment of hypertension and its ability to prevent the sequelae of this silent killer, which include heart attacks, strokes, heart failure, kidney disease, peripheral artery disease, and others, according to The Surgeon General’s Call to Action to Control Hypertension (2020).
Marvin Moser, a leading hypertension researcher who passed away in 2017, wrote about what it was like dealing with hypertension during and after World War II.
“Those of us who were house staff officers in the 1940s recall that every third or fourth medical bed was occupied by sick, middle-aged patients with some complication of hypertension—heart failure, stroke, accelerated hypertension, or renal failure. Yet in 1941, in the first edition of the ‘gold standard’ pharmacologic textbook by Drs. Goodman and Gilman, the only references to hypertension or its therapy … in a volume of more than 1300 pages … were thiocyanates, barbiturates, bismuth, and bromides. Potassium thiocyanate was introduced in 1940 to treat hypertension but was relatively ineffective at the dosages used and had many potential side effects. Similarly, barbiturates, bismuth, and bromides were mainly supportive rather than therapeutic in nature and were used along with lifestyle measures—rest and avoidance of stress (both emotional and physical).”
We know today that hypertension is the leading preventable risk factor for cardiovascular disease and all-cause mortality worldwide. The global incidence and prevalence of hypertension and, more importantly, its cardiovascular complications have not decreased despite extensive knowledge about both prevention and treatment options. This is partially due to shortcomings in the early detection, diagnosis, and management of the disorder in an aging global population.
Here are some basic facts about high blood pressure in the U.S.
Having hypertension puts you at risk for heart disease and stroke, which are leading causes of death in the United States.
In 2021, hypertension was a primary or contributing cause of 691,095 deaths in the United States.
Nearly half of adults have hypertension (48.1%, 119.9 million), defined as a systolic blood pressure greater than 130 mmHg or a diastolic blood pressure greater than 80 mm Hg, or are taking medication for hypertension.
About 1 in 4 adults with hypertension have their hypertension under control (22.5%, 27.0 million).
About half of adults (45%) with uncontrolled hypertension have a blood pressure of 140/90 mm Hg or higher. This includes 37 million U.S. adults.
All adults with hypertension are recommended to undergo lifestyle modifications. This is the only treatment recommendation for 1 in 5 adults (25.0 million).
Most adults with hypertension (4 in 5) are also recommended to take prescription medication (94.9 million).
Many adults who are already treated with antihypertensive medication(s) may need to have their current medication dosage increased or to be prescribed additional medications to achieve blood pressure control (33.2 million). More than half of this group have blood pressure ≥140/90 mm Hg (18.8 million).
Many adults for whom hypertension medication is recommended are untreated (34.8 million). Two-thirds of this group have blood pressure of ≥140/90 mm Hg (23.4 million).
High blood pressure costs the United States about $131 billion each year, averaged over 12 years from 2003 to 2014.
The problem with preventing the consequences of high blood pressure is that it has to be detected, treated, and then controlled.
Let’s look at hypertension globally. First, it is the leading risk factor for preventable deaths
Data from "Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990--2016" in The Lancet and WHO.
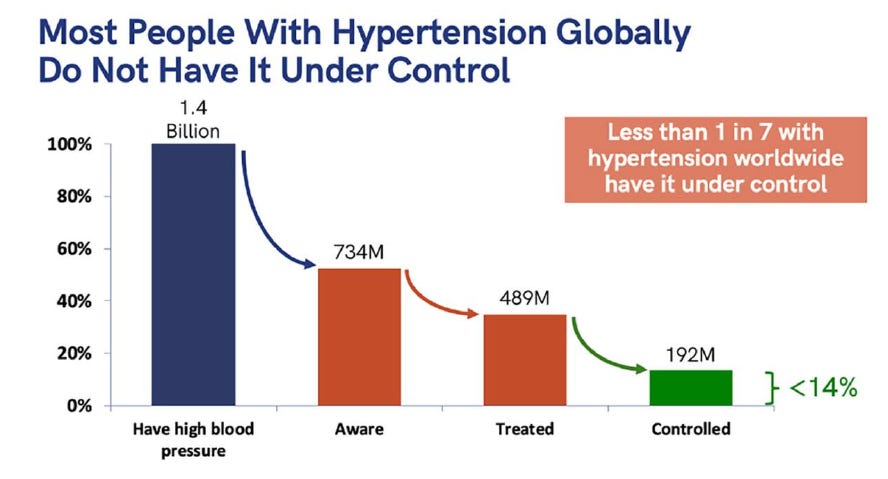
Secondly, similarly to the U.S., most people worldwide do not have their hypertension controlled.
So why, after all this time knowing how to detect, treat, and control high blood pressure, are the numbers so poor? Here are the hurdles to controlling blood pressure, according to Resolve to Save Lives, whose CEO and Director is Dr. Tom Frieden.
According to several experts (Willie M. Abel, PhD, Keith C. Ferdinand, MD, Naomi D.L. Fisher, MD, and Carl J. Pepine, MD) drastic actions are needed to combat rising hypertension rates and worsening control. They recommended that a fundamentally different approach to treating patients with hypertension is required. Hypertension care should be multidisciplinary and team-based and involve patient self-management education, remote monitoring, coaching, and long-term management of a chronic condition.
Both genetic and environmental factors lead to hypertension. Environmental causes are the most important. Unhealthy diets and the obesity pandemic contribute directly to raising blood pressure. High blood pressure is linked to increased sodium, alcohol, and poor potassium intake. Our modern lifestyle of eating out more, preparing less, and having less time bolsters these links and leads to worsening cardiovascular health. There are those who contend that the abundance and types of foods around us make diet control daunting.
The U.S. Preventive Services Task Force and the American Heart Association recommend taking blood pressure measurements at home to confirm the diagnosis before starting treatment, but most hypertension is diagnosed and treated based on doctor’s office BP measurements. So remote management is where we should be headed. Adherence and BP management will improve if individuals believe it is necessary to control their BP and use provided home BP monitors to track their BP throughout the day.
The hypertensive patient needs to be an active partner. Collaborative decision-making is the most crucial hypertension control technique, even with new classes of drugs. Most patients need two or more therapies to reduce BP, along with lifestyle changes. Hypertension management requires more resources, effort, and personnel.
We need all the aforementioned strategies to improve blood pressure awareness, treatment, and control. But we also need to consider the environment we live in. In the Five Insights from the Global Burden of Disease Study 2019, one conclusion is that relying on individuals alone rather than government help makes addressing a public health problem much more difficult. The authors state that this concept is naïve since environment, education, and life options vary greatly from one person to another, influencing health or prevention choices. Governments should help everyone make healthier choices. To preserve public health, government regulation, taxation, and subsidies may be needed just like they were for tobacco control.
The Lancet Commission on Hypertension addressed four problems with hypertension management, providing goals and actions to address each in their paper, “A call to action and a lifecourse strategy to address the global burden of raised blood pressure on current and future generations”. One problem was exposure to an unhealthy environment. Their goal was to develop collaborations between government and non-government organizations to create a healthy environment. They proposed exploring and adopting integrated, unified methods and policies to accelerate health-promoting conditions, such as making it easier to choose healthy foods, discouraging unhealthy ones, and increasing physical exercise. Here is what the World Heart Federation says about diet as part of a larger infographic.
These worthy goals and proposals for the world to address hypertension call for the individual, the healthcare system, the government, and other entities to play a role in a team approach to managing hypertension. Some of these goals are formidable. But we should try to help individuals by somehow changing the food environment we all live in.
Let me close with a reflection from Dr. Edward Freis, a pioneer in prevention. He organized the first double-blind randomized controlled trial comparing single agents and combination medicines in hypertension, showing the advantage of antihypertensive medications for avoiding cardiovascular damage in moderate to severe hypertension patients.
Following the success of this trial, Freis directed cooperative hypertension investigations, advocated for antihypertensive medication in all patients, and became one of the world's leading hypertension experts.
As Dr. Freis said,
“The VA [Veterans Affairs] Cooperative Study will be remembered for changing the management of hypertension. It altered the emphasis from secondary forms of hypertension, which while still important, applied only to a small percentage of the hypertension population. It convinced physicians that the numerically much more prevalent essential or primary hypertension could be benefited by antihypertensive drug treatment. Our study demonstrated that by controlling the blood pressure, we could prevent most of the complications of the disorder, and equally important, its progression to a more severe state could be arrested.”
We can and must do more. Think of the impact on preventing death and disability, let alone the financial payback, if we could improve the detection, awareness, treatment, and control of hypertension, the world’s leading killer.